Streamlined RCM Tailored for
Physical Therapy Clinics
Physical Therapy Subspecialties Billing Services
Ambula provides comprehensive billing services for all physical therapy subspecialties. Whether it’s orthopedic, neurological, pediatric, geriatric, cardiopulmonary, sports, or women’s health physical therapy, Ambula ensures accurate claim submission, compliance, and efficient revenue cycle management.

*Results may vary
Acceptance Rate*
Additional Collection*
Product Quality Index
Energy Generation
Explore Business Specific Revenue Cycle Management Services
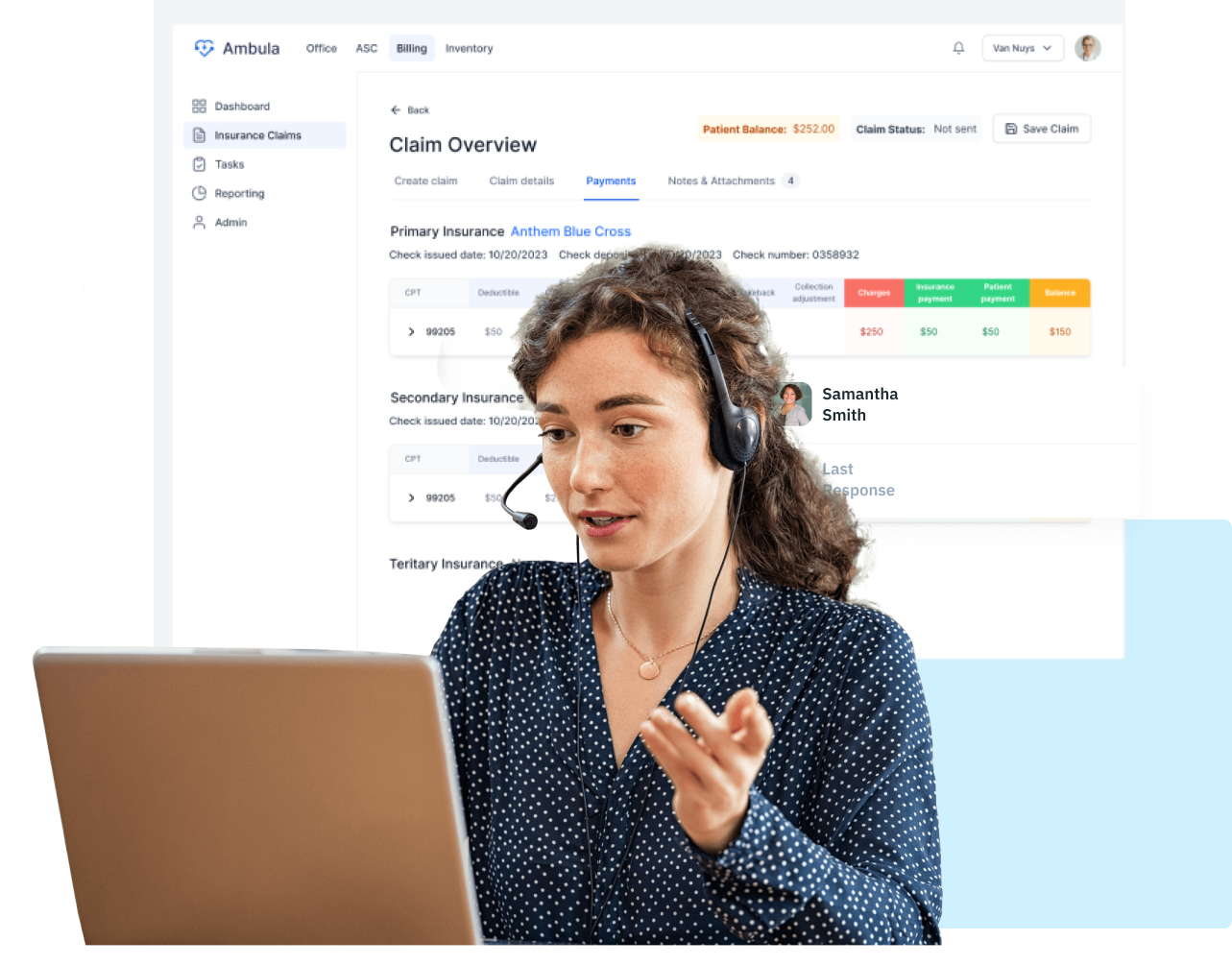
Everything you need in one place
Our process makes sure patients are brought on board, treatments are recorded with the right medical codes, claims are filed , claim statuses are watched , payments are recorded , and claim rejections are solved fast. This full approach boosts revenue to the max, keeps everything in line with rules, and makes the money flow smoother for physical therapy practices.

Why to Choose Ambula Billing Service?
Pick Ambula to handle your physical therapy billing. We make sure claims are submitted , follow HIPAA rules, and deal with denials . We know ICD-10 and CPT codes inside out, send claims , and post payments fast. This means more money for you and smoother billing overall. Let Ambula take care of signing up patients, checking insurance, and keeping records. We’ll keep your practice running well and making money.
Share your wedding moments with your guests
Ambula RCM
Simplify Orthopedic Revenue Cycle Management (RCM)
End-to-end solutions to maximize collections and streamline your orthopedic practice.
Optimize Billing Processes
Ensure accurate and timely billing for personal injury cases, reducing delays and increasing revenue.
Seamless Attorney Collaboration
Leverage our integrated network of attorneys and case managers for efficient case management and faster payments.
Claim and Lien Tracking
Stay updated on claim statuses with intuitive tracking tools that eliminate manual work.
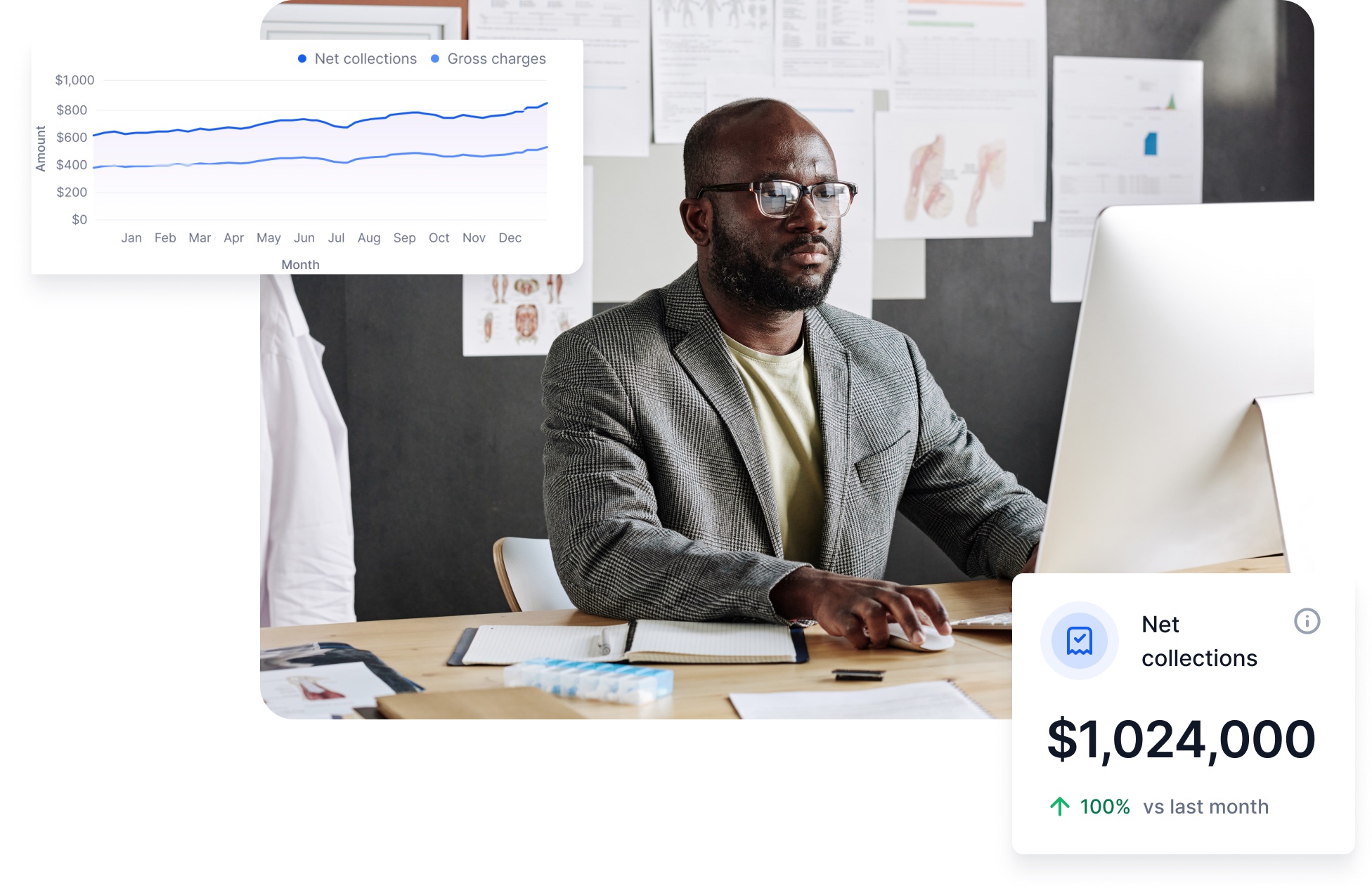
Customized Reporting
Gain insights into your clinic’s financial performance with detailed, customizable reports.
Frequently asked questions
Everything you need to know about the Billing service