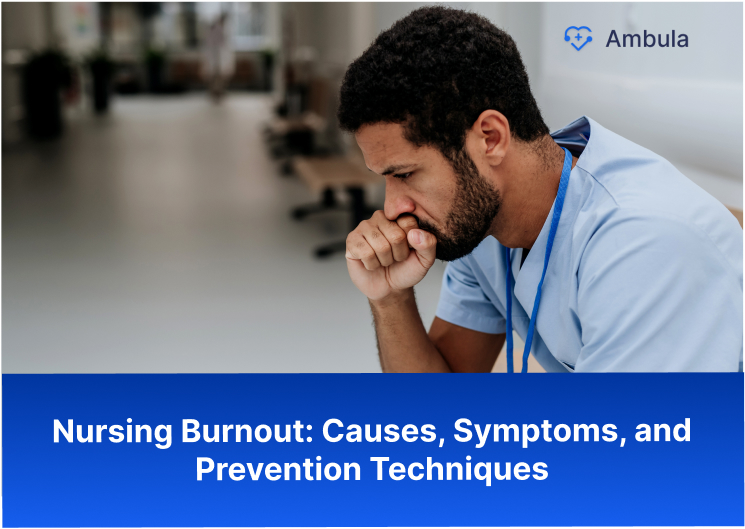
Navigating a nursing career means encountering the reality of burnout. Recognizing it is as crucial as any skill you’ve mastered. Recent studies show that up to a third of nurses face burnout, which can compromise personal well-being and patient care quality.
Burnout goes beyond stress—it can sap your drive and leave you feeling empty inside. It affects physical health, job satisfaction, and social life. Knowing the causes, symptoms, and prevention strategies is key to maintaining the high standards of care that define nursing.
Nursing Burnout Definition
The definition of nursing burnout refers to a state of physical, emotional, and mental exhaustion experienced by nurses due to prolonged stress and high demands in the workplace. It is a condition characterized by overwhelming anxiety, fatigue, and dissatisfaction with one’s job and career.
Check out these articles after you’re done
- How nurses benefit from a surgery center EHR?
- Causes of physician burnout and tips for prevention
- Strategies for reducing doctor burnout in the workplace

Why is Burnout so Common in Nursing?
The high prevalence of burnout among nurses is due to several factors, including long hours, heavy workloads, and exposure to stressful and traumatic situations. Nursing is physically and emotionally demanding, and nurses are often required to work long shifts and care for patients in sometimes life-or-death cases. These demands can take a toll on even the most dedicated and compassionate nurses.
In addition to the physical and emotional demands of the job, nurses also face numerous organizational and structural factors that contribute to burnout. These factors include a lack of autonomy, insufficient staffing, and inadequate support and resources.
Moreover, many nurses also face emotional and moral distress, which can further contribute to burnout. This distress may arise from ethical conflicts, such as being required to provide care that is at odds with their values or from witnessing the suffering of their patients and their families.
These physical, emotional, and organizational factors explain why burnout is so common in nursing. To address this issue and improve the well-being of nurses, healthcare organizations need to take steps to reduce the risk of nurse burnout and provide adequate support and resources to those affected.
The Prevalence of Burnout in Nursing
You’ve likely heard the buzzword “burnout” being tossed around in breakrooms and during shift changes. It’s not just jargon; the struggle is real and it’s widespread across the nursing profession. So, let’s unpack the numbers to get a clearer image.
A staggering 40% of hospital nurses have reported experiencing symptoms of high burnout. That means nearly half the folks you pass in the corridor might be silently grappling with it. Considering the tight-knit fabric of the nursing community, this statistic isn’t just a number—it’s a reflection of the well-being of your peers.
In some specialties, the rates are even higher. For instance, critical care units see a burnout rate that can hover around 50%, which isn’t surprising given the intense nature of the work. These figures place nursing among the top professions for burnout prevalence, standing shoulder-to-shoulder with other high-stress fields like emergency responders and social workers.
The long hours and the emotional rollercoaster that comes with patient care contribute to these figures. Picture this: a 12-hour shift with back-to-back critical tasks, where the only sit-down moment you get is when documenting care. Then multiply that by three or four days a week—it adds up, doesn’t it?
If you constantly run on empty before the next shift starts, know you’re not alone. This isn’t the norm just for seasoned veterans; newbie nurses fresh out of school are also thrust into this reality early on. It’s a clear sign that the prevalence of burnout isn’t just about individual stamina—it’s a systemic issue in the healthcare field.
Root Causes of Nursing Burnout
You’re powering through your shift, juggling patient care, endless paperwork, and the occasional emotional moment with families. Ever wonder why the flame of passion for nursing seems to flicker sometimes? It’s not just the long hours. If you dig deeper, you’ll find the root causes of nursing burnout; it’s a mix of systemic issues and enervating work conditions.
Firstly, consider the high patient-to-nurse ratios. You’re shouldering the health and well-being of more lives than can sometimes be feasibly managed within the constraints of your shift. Ever feel like you’re being pulled in a dozen different directions, yet, at the end of the day, can’t shake the feeling that you haven’t done enough? When there are too many patients and not enough nurses to go around, the quality of care can be compromised, and that nagging sense of inadequacy creeps in.
Now, factor in the emotional toll. Nursing isn’t just a job; it’s an emotional journey. You’re there for some of a person’s most intimate and impactful moments. Bearing witness to suffering, illness, and sometimes loss takes a hefty emotional toll that can accumulate stealthily.
Understaffing exacerbates the problem. With not enough hands on deck, you’re often expected to do more with less—less time, less support, and fewer resources. It’s like being in a boat taking on water; no matter how fast you bail it out, you’re still sinking.
Lack of autonomy and a supportive work environment can also contribute to burnout. Feel like your voice goes unheard? When suggestions are ignored, and decisions are made without considering your front-line experiences, it’s eroding—not just your morale but your entire professional enthusiasm.
And let’s not forget the ever-looming shadow of paperwork and administrative tasks. They pile up, don’t they? Subtract the hours spent on documentation and indirect patient care, and what you’re left with can feel like mere snippets of actual nursing.
It’s a complex blend, right? Overwork, emotional strain, understaffing, and feeling undervalued—each a thread in the tapestry of nursing burnout. Recognizing these root causes is empowering. With clarity comes the power to advocate for change, both on the ground and at the policy level. As you stand on the front lines of healthcare, understanding these factors is crucial in the collective push toward a sustainable and fulfilling nursing career. Remember, you’re not just the backbone of healthcare—you are its heart and soul. And that deserves an environment where you can thrive, not just survive.
Symptoms and Warning Signs of Burnout
Hey there, let’s chat about something you’ve probably brushed shoulders with more often than you’d like: the warning signs of burnout. Recognizing these can be tricky. They’re often subtle, creeping up on you over time until you realize you’re not feeling quite like your usual, energetic self.
You may start noticing a nagging exhaustion not cured by a good night’s sleep. It’s like you’ve hit a wall of fatigue, and no amount of coffee is seeing you through your shift. This isn’t just “tired” — it’s a profound physical and emotional depletion.
Then, there’s the mental distance. Maybe you’re feeling a bit more cynical about work, or perhaps you are less empathetic towards patients. It might feel like you’re just going through the motions, detached and disengaged — a protective shell that might help in the short term but can be a red flag.
Your job performance might start to wobble, too. Those small mistakes you wouldn’t typically make become more frequent, or you’re not as quick on your feet when making decisions. If you’re leaving each shift feeling like you haven’t made a real difference, that sense of professional inefficacy can be a glaring symptom of burnout.
On top of that, you might notice changes in your health. Are headaches becoming a regular nuisance? Maybe your appetite isn’t what it used to be, or stomach issues are suddenly on the rise without a clear cause. These can all be subtle signs your body is waving a white flag.
Personal Strategies for Preventing Burnout
Self-care is fundamental. Prioritize downtime and nourish your body with satisfying breaks and quality sleep, aiming for 7-8 hours a night. Set boundaries to avoid overcommitting – your well-being is vital, and turning down extra shifts to protect it is okay.
Cultivate a support network of peers for mutual encouragement. A shared laugh or understanding nod can make a difference on a tough day. Keep hobbies and passions alive; they’re not just pastimes. They’re lifelines to personal fulfillment.
Incorporate mindfulness into your daily routine. Just a few minutes can center your thoughts and reduce stress. And if you’re shouldering too heavily, seeking professional support is a step toward resilience, not a sign of weakness.
Adopting these focused strategies, you maintain professional compassion without compromising your health. Remember, a well-balanced nurse is a force of care and capability.
Organizational Strategies to Prevent Burnout
Smart staffing ratios are key—sufficient personnel reduces overtime and supports work-life balance. Encourage open communication; leaders must actively listen and respond, indicating staff voices matter.
Foster professional development. Providing educational and advancement opportunities motivates and shows investment in staff careers, which can keep daily duties from feeling monotonous.
Create a supportive atmosphere with simple morale boosters like recognition programs. These gestures enhance team spirit and show appreciation for hard work.
Implement flexible scheduling to honor nurses’ needs outside the workplace, demonstrating respect for their time.
These targeted strategies help build a workplace where nurses can flourish, improving care quality and strengthening the healthcare system.
Effects of Nursing Burnout
The effects of nursing burnout can be far-reaching, impacting not only the nurse but also their colleagues, patients, and the healthcare system. Some of the impacts of nursing burnout include:
- Decreased job satisfaction and increased job turnover
- Reduced job performance and increased absenteeism
- Adverse effects on patient care
- Increased healthcare costs
- Decreased job satisfaction and morale among colleagues
Nursing Burnout Prevention
Preventing nurse burnout is essential to improving the well-being of nurses and the quality of patient care. Some strategies for avoiding nurse burnout include:
- Increasing staffing levels to reduce workloads and avoid overuse
- Improving work-life balance through flexible scheduling and time off
- Providing opportunities for professional growth and development
- Fostering a positive work environment that values and supports its employees
- Encouraging self-care and stress management techniques
- Offering regular burnout prevention and management training
The Role of Leadership in Combating Burnout
Healthcare leaders, note that your actions can directly influence whether burnout becomes a common enemy or a rare exception. Good leadership might be the lynchpin in safeguarding your team’s well-being.
First off, recognition goes a long way. By celebrating your team’s wins and acknowledging their hard work, you’re not just boosting morale—you’re building loyalty and job satisfaction.
Next, you’ve got to mean it when you communicate. When sharing decisions or policy changes, transparency is crucial. Creating an environment where feedback is not just welcomed but actively sought and acted upon fosters a sense of belonging and control among nurses over their work lives.
Provide practical support, too. This means ensuring the tools and resources nurses need to do their jobs effectively are always on hand. Overlook this, and you risk leaving your staff helpless amidst growing demands.
Investing in your team’s professional development has a double pay-off: it can reduce feelings of stagnation and spark a rejuvenating sense of career progression. Whether through mentoring or advanced training programs, show your nurses their growth is a priority.
Conclusion
Nurse burnout is a growing concern in the healthcare industry, and it is essential to address it to improve the well-being of nurses and the quality of patient care. By implementing solutions such as increasing staffing levels, improving work-life balance, and providing opportunities for professional growth, organizations can help prevent and manage nurse burnout and create a healthier work environment.