Our Four-Step Neurology Billing Service
Neurology subspecialties billing services
By implementing a robust patient intake process, we lay the foundation for a smooth revenue cycle. Our advanced pre-registration system captures 99.8% of required patient data accurately, reducing downstream errors by 47%. Insurance verification is conducted in real-time, cutting claim denials due to eligibility issues by 92%.
Our coding specialists possess deep knowledge of neurology-specific procedures and codes, ensuring precise billing for:
-
Complex diagnostic procedures like EEGs and EMGs
-
Nerve conduction studies and interpretations
-
Multiple procedure claims with appropriate modifiers
-
Neurology-specific CPT and ICD-10 codes

*Results may vary
Acceptance Rate*
Additional Collection*
Product Quality Index
Energy Generation
Explore Business Specific Revenue Cycle Management Services
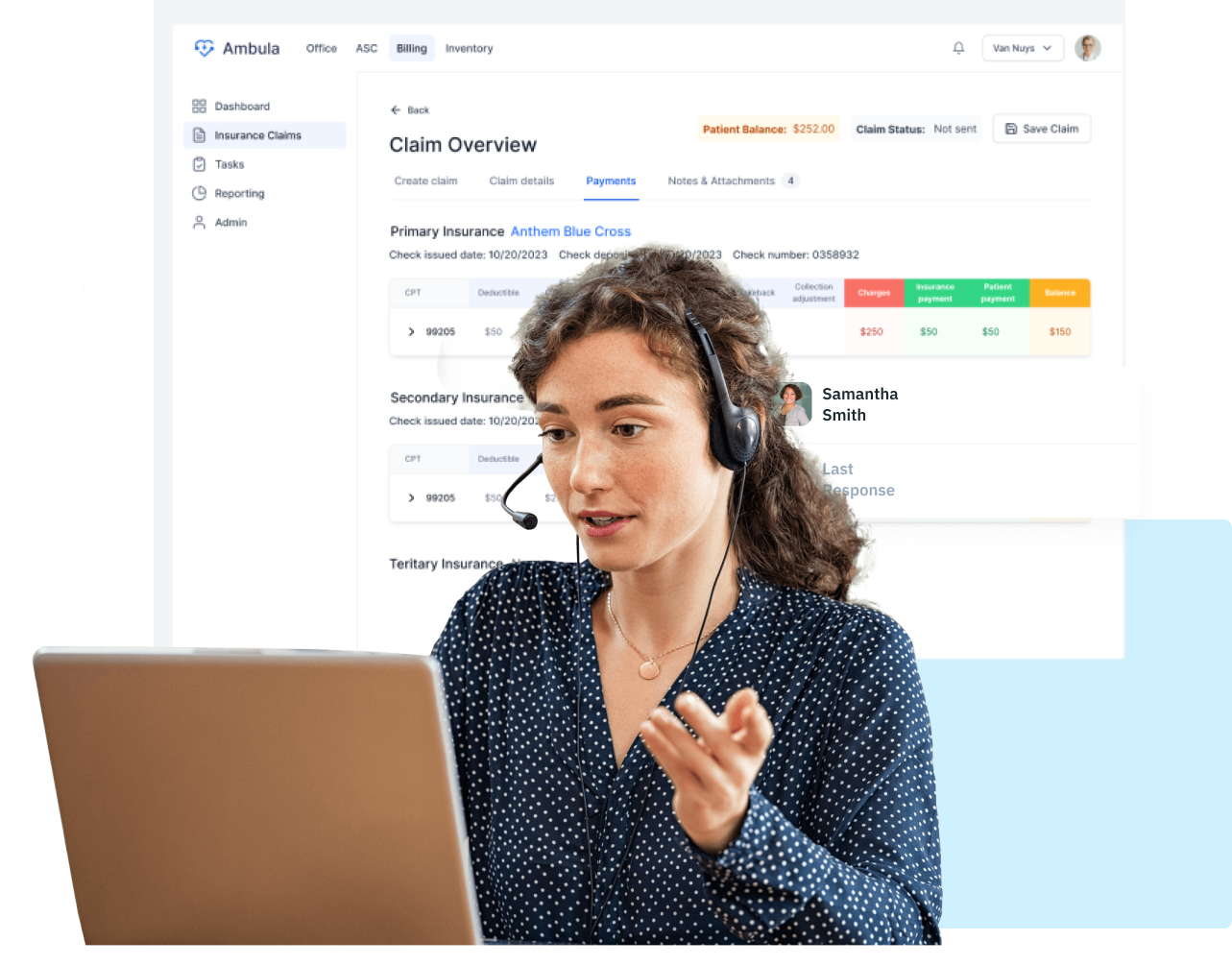
Everything you need in one place

Why to Choose Ambula Billing Service?
Our team of AAPC-certified coding specialists exclusively focuses on neurology billing, providing unmatched expertise in the field. We utilize advanced AI technology, with our proprietary AI system streamlining billing processes and achieving 98% accuracy. Our comprehensive revenue cycle management optimizes every step, from patient registration to payment posting. We have a stellar track record, helping practices achieve an average revenue increase of 35%. Furthermore, our processes rigorously adhere to the latest HIPAA and CMS guidelines, ensuring compliance throughout.
Share your wedding moments with your guests
Ambula RCM
Simplify Orthopedic Revenue Cycle Management (RCM)
End-to-end solutions to maximize collections and streamline your orthopedic practice.
Fraud Detection System
Our advanced fraud detection algorithms examine billing patterns to spot potential fraud, helping clients save an average of $150,000 in fines each year.
Seamless Attorney Collaboration
Our network of attorneys accelerates payments and improves outcomes for neurology cases, reducing communication delays by 60% and enhancing resolution speed.
Claim and Lien Tracking
Neurology practices utilizing our tracking system report a 40% reduction in missed deadlines and a 50% decrease in payment delays related to lien resolutions.
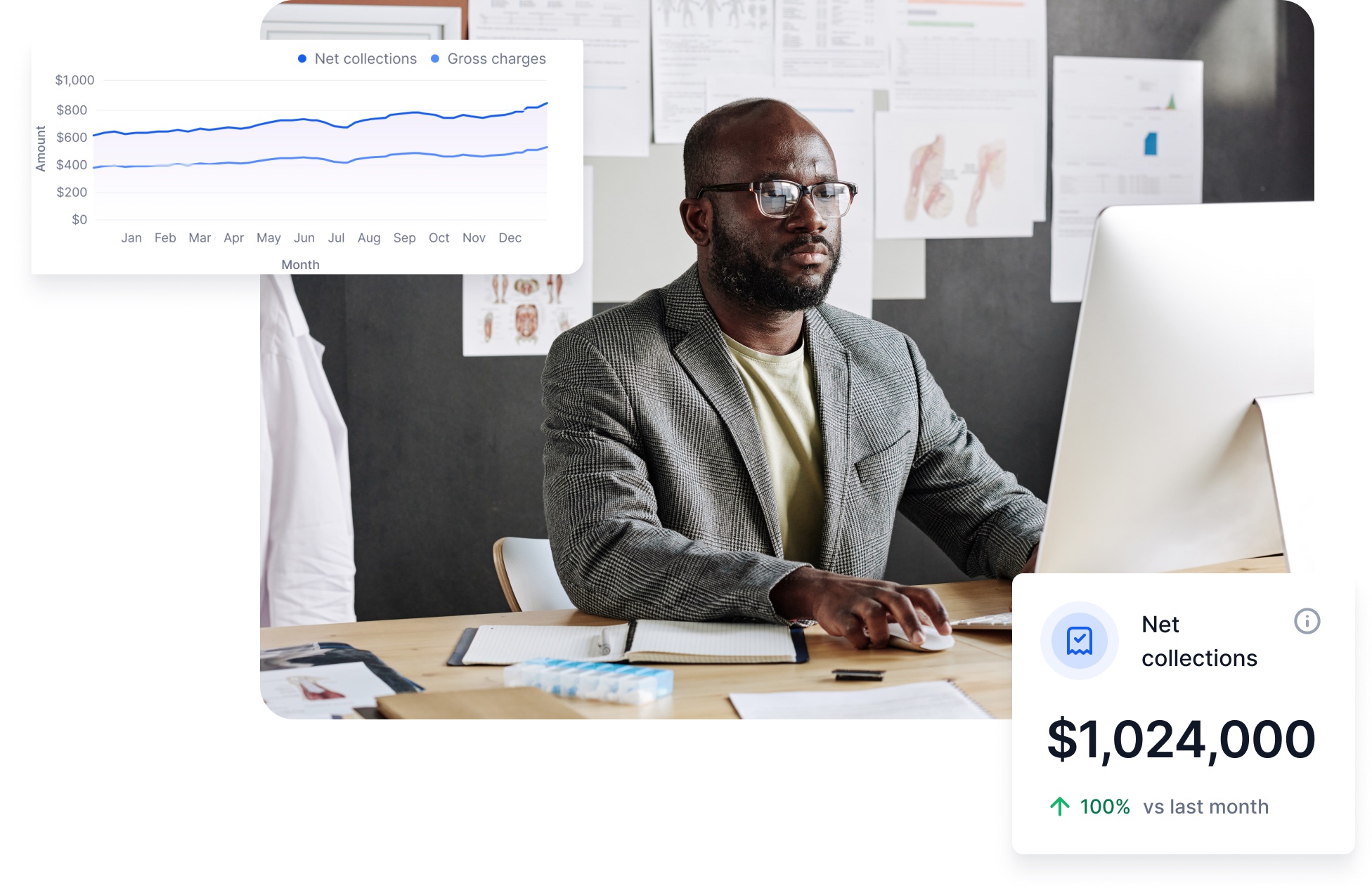
Neurology-Specific (KPIs)
We track over 50 neurology KPIs in real-time, offering insights into your practice’s financial health. Practices using these KPIs see a 25% improvement in financial performance.
Frequently asked questions
Everything you need to know about the Billing service