
Converting EHR systems (Electronic Health Records) is essential for healthcare organizations aspiring to digitize their services, align with federal and state mandates, improve quality of care, and manage structured data more efficiently. However, this process comes with legal and regulatory challenges that can impact the cost of care and the implementation of Health IT Solutions. This post will delve into these and how healthcare providers can navigate them.
Understanding EHR Systems and the Role of Federal and State Mandates
EHR Systems, known as Electronic Health Records, are integral to healthcare organizations. They are designed to improve the quality of care and patient outcomes, simplify data management, and promote health equity. These digital health records take precedence over traditional paper-based systems due to improved data accessibility, patient-doctor communication, and precise medical documentation.
Federal and state mandates further necessitate the need to implement these systems. CMS (Centers for Medicare & Medicaid Services) and other regulatory bodies have been instrumental in shaping the adoption of EHR systems. CMS encourages the adoption through its Meaningful Use and EHR Incentive Programs—initiatives aimed at incentivizing healthcare providers to employ EHR systems effectively.
However, these mandates can also present challenges for healthcare organizations during the conversion process. Complying with the extensive regulations often requires significant investment and strategic planning, making the process daunting for many.
Assessing the Cost of Care and ROI in the EHR Conversion Process
Converting to EHR systems can significantly impact the cost of care, especially for smaller healthcare providers grappling with budget constraints. EHR adoption involves costs such as purchasing the software, implementing Health IT Solutions, training staff, and addressing unforeseen technical issues. Additionally, there may be ongoing costs related to software updates, system maintenance, and IT support.
However, healthcare providers must also consider the return on investment (ROI) offered by EHR systems. EHRs can improve patient care, streamline workflows, and facilitate data exchange between healthcare organizations with proper implementation. These benefits can potentially outweigh the costs in the long run.
Evaluating the ROI also involves analyzing the EHR replacement market. When healthcare organizations transition from legacy EHR systems to first-generation EHRs, they must consider the long-term benefits and costs. Return on investment shouldn’t just be viewed in financial terms alone but also in terms of productivity gain, operational efficiency, and improvements in quality of care.
Addressing Legal and Organizational Challenges
Transitioning to EHR systems raises legal and organizational challenges, such as patient privacy, data security, and compliance with the Health Insurance Portability and Accountability Act (HIPAA). These systems must maintain stringent security protocols to prevent unauthorized access or breaches. Legal liabilities related to patient privacy and data breaches present significant concerns for healthcare organizations.
Acquiring stakeholder consensus is another significant organizational hurdle. Multiple parties, including physicians, nurses, administration, and IT staff, are involved, and ensuring everyone is on board with the system change is critical. This calls for transparency, effective communication, and inclusive decision-making during the EHR conversion process.
Interoperability challenges further amplify the complexities around EHR conversions. EHRs must be selected and implemented to ensure they can interact and exchange data effectively with other systems within and across healthcare organizations. Failing to do so may undermine the system’s efficiency and effectiveness.
Role of Health IT Solutions in EHR Conversion
Health IT solutions can be crucial in ensuring successful EHR conversion by mitigating many of the technical, financial, legal, and organizational challenges associated with the process.
Moving Forward
Ensuring a successful EHR conversion is no small task, but with effective planning and a comprehensive understanding of the legal, financial, and technical challenges, healthcare organizations can significantly improve their quality of care while achieving compliance with federal and state mandates. Ultimately, the aim should be an enhanced patient experience, improved treatment outcomes, and a smoother, more efficient operational process.
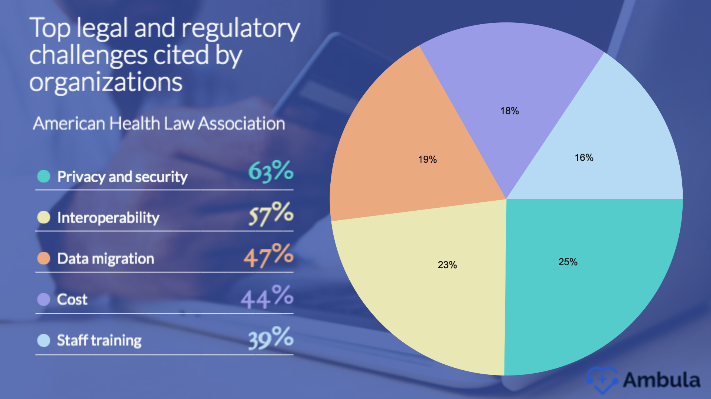
A study by the American Health Law Association found that the top legal and regulatory challenges cited by organizations converting EHRs were:
-
- Privacy and security (63%)
- Interoperability (57%)
- Data migration (47%)
- Cost (44%)
- Staff training (39%)
- Another study by the National Law Center on Health Care Reform found that the average cost of converting to an EHR system is $1.5 million for small practices and $10 million for large hospitals.
- The same study found that the average time to complete an EHR conversion is 2 years.
These data show that the legal and regulatory challenges in converting EHRs can be significant. However, the benefits of EHRs, such as improved patient care and reduced costs, can outweigh the challenges.
Here are some additional data about the legal and regulatory challenges in converting EHRs:
- The Health Insurance Portability and Accountability Act (HIPAA) requires healthcare organizations to protect the privacy and security of patient health information. This can be a challenge when converting EHRs, as organizations must ensure the new system meets HIPAA requirements.
- The Office of the National Coordinator for Health Information Technology (ONC) has developed a set of standards for EHR interoperability. These standards are designed to make it easier for different EHR systems to communicate with each other. However, not all EHR systems comply with ONC standards, making it difficult to achieve interoperability.
- The cost of converting EHRs can be significant, especially for small or rural healthcare organizations. Several government programs offer financial assistance for EHR conversion, but these programs may not be available to all organizations.
- Staff training is essential for the successful implementation of an EHR system. Healthcare staff must be trained to use the new system to ensure that patient care is not interrupted. However, staff training can be a time-consuming and expensive process.
Despite the challenges, the benefits of EHRs can outweigh the risks. EHRs can improve patient care, reduce costs, and improve the efficiency of healthcare organizations. Organizations that are considering converting EHRs should carefully weigh the risks and benefits before making a decision.
Financial Considerations
The financial aspect of EHR conversion can be daunting. Costs associated with new EHR systems can potentially exceed initial estimates due to unforeseen implementation challenges or additional feature requirements. On the other hand, healthcare providers might miss out on potential EHR incentive programs if they don’t implement these systems correctly.
Furthermore, while EHR systems can improve care, increase efficiency and potentially influence reimbursement rates favorably, these results are not guaranteed. Healthcare organizations must thoroughly analyze potential financial risks and devise a sustainable investment strategy for EHR transition.
Addressing Technical Challenges
The technical aspects of converting EHR systems are another significant challenge for healthcare organizations. Data migration, system interoperability, and the choice between Application Service Providers (ASPs) or Software as a Service (SaaS) solutions are some of the critical decisions to navigate in EHR conversion.
Data migration involves moving existing health records from legacy systems to the new EHR platform. This transition must be accomplished without data loss or corruption and with minimum disruption to care services. Poorly executed data migration can result in functional shortcomings of the EHR system and prolonged system downtime.
The choice between ASPs and SaaS can also pose a challenge. While ASPs might provide more customization options, SaaS solutions often offer greater scalability and lower upfront costs. Healthcare organizations must carefully evaluate their needs and constraints before deciding on the best model.




