Medical offices face 5 major challenges that impact their efficiency: increasing patient volumes, complex insurance requirements, staffing shortages, regulatory compliance demands, and evolving technology. These challenges create bottlenecks that affect both patient care and staff satisfaction.
To improve workflow in medical office settings, practices must first recognize that optimized workflows directly impact 3 critical areas: patient satisfaction, staff productivity, and financial performance. A study by the Medical Group Management Association found that practices with optimized workflows saw a 30% reduction in patient wait times and a 25% increase in daily patient volume without adding staff.
Medical office workflow optimization isn’t just about moving faster—it’s about working smarter. When processes flow smoothly, medical staff spend less time on administrative tasks and more time on patient care. This shift not only improves clinical outcomes but also enhances the work environment, reducing burnout and turnover rates among healthcare professionals.
The financial impact of streamlined medical office processes is equally significant. Efficient billing workflows reduce claim denials, while optimized scheduling minimizes gaps in the appointment calendar. Together, these improvements can increase practice revenue by up to 15%, according to healthcare consulting firm Advisory Board.
Mapping and Analyzing Current Workflows
healthcare workflow improvement (secondary keyword): Effective Healthcare Workflow Improvement Begins with Process Mapping
Healthcare workflow improvement starts with a thorough analysis of current processes. Before making changes, medical offices must document exactly how work flows through their practice today. This mapping process reveals inefficiencies that might otherwise remain hidden.
To map your current workflow, follow these 7 specific steps:
- Identify all major processes (check-in, examination, billing, etc.)
- Document each step within these processes
- Note who performs each step and how long it takes
- Identify handoffs between staff members
- Record technology used at each stage
- Document decision points and variations
- Note pain points reported by staff and patients
When mapping workflows, involve staff from all departments. Front desk personnel, medical assistants, nurses, providers, and billing specialists each bring unique perspectives on where bottlenecks occur. Their input is invaluable for identifying problems that might not be obvious from management’s viewpoint.
After mapping current processes, analyze the data to identify specific improvement opportunities. Look for these 5 common inefficiencies:
- Redundant steps where the same information is recorded multiple times
- Bottlenecks where work piles up waiting for a specific person or resource
- Unnecessary handoffs between staff members
- Paper-based processes that could be digitized
- Tasks that frequently cause errors or delays
This analysis forms the foundation for all subsequent improvement efforts. Without understanding your current state, attempts to streamline medical office processes may address symptoms rather than root causes.
Technology Integration for Workflow Enhancement
EHR workflow integration (secondary keyword): Optimizing EHR Workflow Integration for Maximum Efficiency
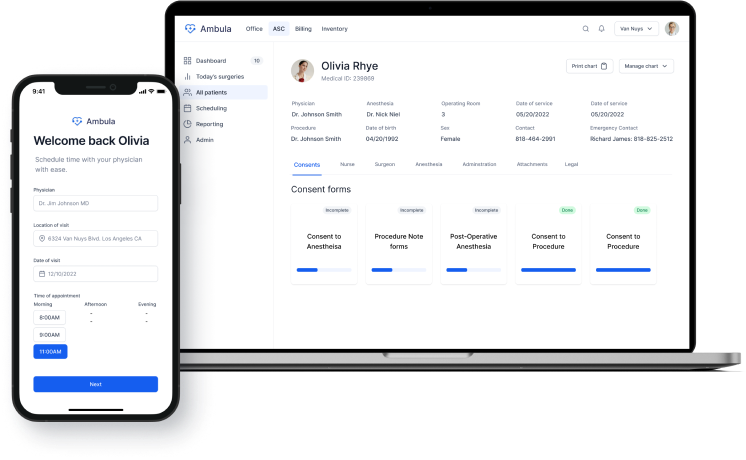
EHR workflow integration represents one of the most significant opportunities to improve workflow in medical office settings. While most practices have implemented electronic health records, many fail to optimize these systems to support efficient workflows. Proper EHR workflow integration can save medical staff hours of documentation time.
To optimize your EHR system, focus on these 4 specific areas:
- Template customization: Create specialty-specific templates that match your practice’s common visit types
- Order set development: Build order sets for frequent conditions to reduce clicks and save time
- Documentation shortcuts: Implement auto-text features and voice recognition to speed note creation
- Role-based access: Configure the EHR to show each user only the functions they need
Beyond EHR optimization, medical offices should consider implementing additional technologies to automate medical office tasks. Digital patient intake solutions eliminate paper forms and reduce data entry errors. These systems allow patients to complete forms before their visit, with information flowing directly into the EHR.
Appointment scheduling and reminder systems represent another area where technology can dramatically improve workflow in medical office environments. Automated appointment reminders reduce no-shows by 30-40%, according to a study in the Journal of Medical Practice Management. Online scheduling options decrease phone call volume, freeing staff for other tasks.
Patient flow optimization (secondary keyword): Patient Flow Optimization Through Digital Solutions
Patient flow optimization benefits significantly from technology integration. Digital check-in kiosks reduce front desk bottlenecks, while patient tracking systems help staff monitor wait times and room utilization. These tools provide real-time data that enables proactive management of patient flow.
For billing workflows, automated eligibility verification and claim scrubbing tools catch errors before submission, reducing denial rates and accelerating payment cycles. These technologies typically deliver return on investment within 6-12 months through improved collections and reduced administrative costs.
Staff Training and Change Management
clinical workflow management (secondary keyword): Effective Clinical Workflow Management Requires Staff Buy-In
Successful clinical workflow management depends on staff engagement and proper training. Even the best-designed workflows fail when staff members don’t understand or accept them. Effective clinical workflow management reduces administrative burden on healthcare providers and improves job satisfaction.
When implementing workflow changes, follow these 6 steps to ensure staff buy-in:
- Involve staff in the design process from the beginning
- Clearly communicate the reasons for change
- Provide comprehensive training before implementation
- Offer additional support during the transition period
- Solicit feedback and make adjustments as needed
- Recognize and celebrate early successes
Training should be role-specific and hands-on. Generic training sessions rarely translate to real-world workflow improvements. Instead, develop training scenarios that mirror actual patient encounters, allowing staff to practice new workflows in a controlled environment.
Change management strategies should address the emotional aspects of workflow changes. Staff members may feel anxious about learning new systems or worry that efficiency improvements could threaten their jobs. Addressing these concerns openly helps overcome resistance.
Documentation plays a critical role in sustaining workflow improvements. Create clear, accessible standard operating procedures (SOPs) for all key processes. These documents serve as training tools for new staff and reference materials for existing team members.
Patient-Centered Workflow Design
patient flow optimization (secondary keyword): Patient Flow Optimization Strategies That Enhance Experience
Patient flow optimization leads to shorter wait times and improved satisfaction. When redesigning workflows, consider the patient journey from scheduling through follow-up care. Each touchpoint offers opportunities to improve both efficiency and patient experience.
Start by mapping the patient journey through your practice, identifying 8 key touchpoints:
- Appointment scheduling
- Pre-visit preparation
- Check-in
- Waiting room experience
- Clinical encounter
- Check-out
- Billing and payment
- Follow-up communication
For each touchpoint, gather patient feedback through surveys, focus groups, or advisory councils. This input reveals pain points that might not be obvious to staff who experience workflows from a different perspective.
To improve workflow in medical office settings while enhancing patient experience, implement these specific strategies:
- Stagger appointment times to reduce waiting room congestion
- Implement “fast track” protocols for simple visits
- Design exam rooms for efficiency with standardized layouts and equipment
- Create clear wayfinding signage to help patients navigate your facility
- Develop protocols for handling common scenarios like late arrivals
Digital communication tools can significantly enhance the patient experience while improving workflow efficiency. Secure messaging platforms allow patients to ask questions without phone calls, while patient portals provide 24/7 access to test results and appointment scheduling.
Measuring Performance and Continuous Improvement
healthcare workflow improvement (secondary keyword): Measuring Healthcare Workflow Improvement Through Key Metrics
Healthcare workflow improvement requires ongoing measurement and adjustment. Without clear metrics, practices cannot determine whether changes are delivering the expected benefits. Effective measurement focuses on 4 key areas: operational efficiency, financial performance, patient satisfaction, and staff experience.
For operational metrics, track these 5 specific indicators:
- Patient wait times (check-in to provider, room to provider, total visit)
- Cycle times for key processes (registration, rooming, provider visit)
- Schedule utilization rate (percentage of available appointments filled)
- No-show and late cancellation rates
- Room turnover times
Financial metrics should include:
- Days in accounts receivable
- Clean claim rate (percentage of claims paid on first submission)
- Cost per visit
- Revenue per provider hour
- Denial rate by reason code
Patient satisfaction metrics typically come from surveys that assess specific aspects of the visit experience. Staff satisfaction surveys should similarly focus on workflow-related factors like time pressure, task distribution, and technology usability.
Data collection should be systematic and ongoing. Many metrics can be extracted from practice management and EHR systems, while others require manual tracking. Dashboard tools that display key metrics in real-time help practice leaders identify and address problems quickly.
The continuous improvement cycle follows 4 steps:
- Measure current performance using established metrics
- Identify opportunities for improvement based on data
- Implement targeted changes to address specific issues
- Measure results and adjust as needed
This cycle never ends—workflow optimization is an ongoing process, not a one-time project. Regular workflow audits, conducted quarterly or semi-annually, help identify new improvement opportunities as practice needs evolve.
Real-World Success Stories
Medical practices across the country have achieved significant results through focused workflow improvement efforts. These case studies illustrate the potential benefits of medical office workflow optimization.
Case Study 1: Primary Care Practice in Colorado
A 5-provider primary care practice implemented digital patient intake and check-in kiosks, reducing check-in time from 8 minutes to 3 minutes per patient. This change allowed them to see 4 additional patients per day without extending office hours, increasing annual revenue by $120,000.
Case Study 2: Orthopedic Specialty Clinic in Florida
This 12-provider practice redesigned their clinical workflows to standardize room setup and equipment placement. They also implemented medical assistant protocols for patient preparation. These changes reduced provider time per visit by 15%, allowing each physician to see 3 additional patients daily.
Case Study 3: Multi-Specialty Group in Texas
By optimizing their EHR templates and implementing automated appointment reminders, this practice reduced no-show rates from 18% to 7%. They also saw a 35% reduction in time spent on documentation, allowing providers to complete charts during regular hours rather than after work.
These examples demonstrate that targeted workflow improvements deliver measurable results. While each practice’s needs differ, the principles of workflow analysis, staff engagement, technology optimization, and continuous measurement apply universally.
Conclusion
Medical office workflow optimization represents a significant opportunity to improve patient care, staff satisfaction, and financial performance. By systematically analyzing current processes, implementing targeted improvements, and measuring results, practices can achieve substantial efficiency gains.
The journey to improve workflow in medical office settings requires commitment from leadership and engagement from staff at all levels. While technology plays an important role, successful workflow improvement depends equally on people and processes.
Ready to transform your medical office workflows? Contact our team for a personalized workflow assessment and implementation plan tailored to your practice’s unique needs.